Degenerative Disc Disease: Symptoms, Causes & Treatment
Degenerative Disc Disease
What is Degenerative Disc Disease?
Between the spinal bones are inter vertebral discs acting like little shock absorbers, cushioning the joints. Over time, ordinary wear and tear takes its toll on these discs. Despite its name, degenerative disc disease is a condition, not a disease. “Degenerative” simply means symptoms get worse over time. Other chronic degenerative diseases include arthritis and macular degeneration.
Degenerative disc disease is one of the most common spinal issues and a leading cause of back and neck pain. While it can be uncomfortable, degenerative disc disease doesn’t usually cause disability, nor should it require surgery or other invasive treatments.
Often, the pain from degenerative disc disease doesn’t get worse because, ironically, as the discs stiffen, they offer more support. In fact, many individuals diagnosed with degenerative disc disease discover that pain and other symptoms subside after a few months, so living with it is doable.
Degenerative Disc Disease Symptoms
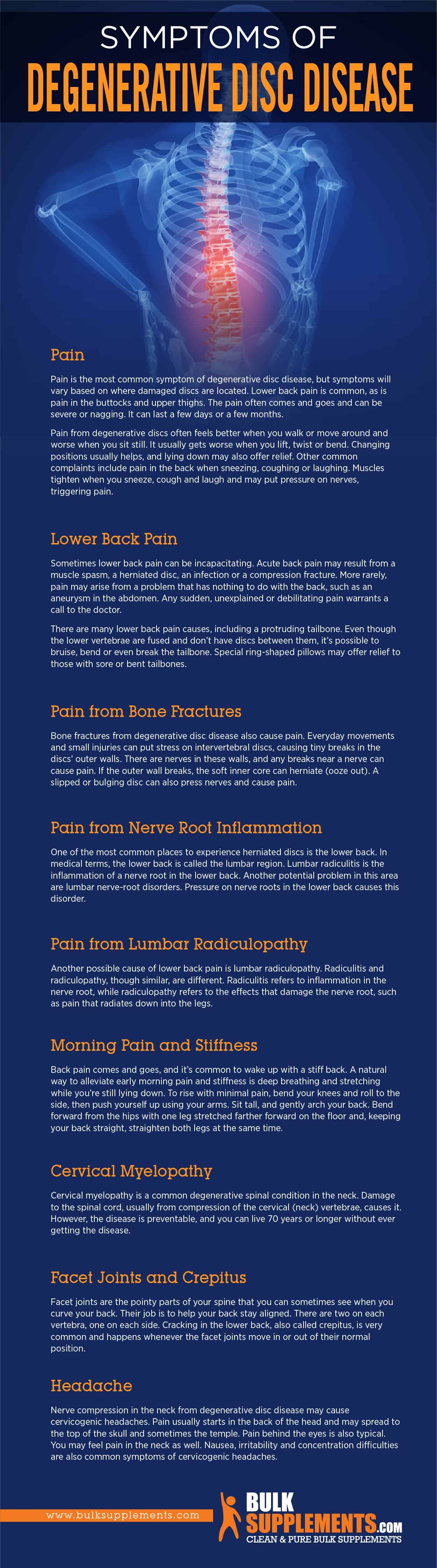
Pain
Pain is the most common symptom of degenerative disc disease, but symptoms will vary based on where damaged discs are located. Lower back pain is common, as is pain in the buttocks and upper thighs. The pain often comes and goes and can be severe or nagging. It can last a few days or a few months.
Pain from degenerative discs often feels better when you walk or move around and worse when you sit still. It usually gets worse when you lift, twist or bend. Changing positions usually helps, and lying down may also offer relief. Other common complaints include pain in the back when sneezing, coughing or laughing. Muscles tighten when you sneeze, cough and laugh and may put pressure on nerves, triggering pain.
Lower Back Pain
Sometimes lower back pain can be incapacitating. Acute back pain may result from a muscle spasm, a herniated disc, an infection or a compression fracture. More rarely, pain may arise from a problem that has nothing to do with the back, such as an aneurysm in the abdomen. Any sudden, unexplained or debilitating pain warrants a call to the doctor.
There are many lower back pain causes, including a protruding tailbone. Even though the lower vertebrae are fused and don’t have discs between them, it’s possible to bruise, bend or even break the tailbone. Special ring-shaped pillows may offer relief to those with sore or bent tailbones.
After the lower back, the neck is the next most common area to experience pain due to wear and tear on the intervertebral discs. While genetics may play a role in degenerative disc disease causing pain in the neck, injury is the usual cause.
Pain from Bone Fractures
Bone fractures from degenerative disc disease also cause pain. Everyday movements and small injuries can put stress on inter vertebral discs, causing tiny breaks in the discs’ outer walls. There are nerves in these walls, and any breaks near a nerve can cause pain. If the outer wall breaks, the soft inner core can herniate (ooze out). A slipped or bulging disc can also press nerves and cause pain.
Pain from Nerve Root Inflammation
One of the most common places to experience herniated discs is the lower back. In medical terms, the lower back is called the lumbar region. Lumbar radiculitis is the inflammation of a nerve root in the lower back. Another potential problem in this area are lumbar nerve-root disorders. Pressure on nerve roots in the lower back causes this disorder.
However, degenerated discs aren’t the only cause of nerve root disorders. Diabetes, tumors, infections such as shingles (herpes zoster) and tuberculosis are other potential causes. You should see a doctor to determine the underlying problem.
Pain from Lumbar Radiculopathy
Another possible cause of lower back pain is lumbar radiculopathy. Radiculitis and radiculopathy, though similar, are different. Radiculitis refers to inflammation in the nerve root, while radiculopathy refers to the effects that damage the nerve root, such as pain that radiates down into the legs.
Morning Pain and Stiffness
Back pain comes and goes, and it’s common to wake up with a stiff back. A natural way to alleviate early morning pain and stiffness is deep breathing and stretching while you’re still lying down. To rise with minimal pain, bend your knees and roll to the side, then push yourself up using your arms. Sit tall, and gently arch your back. Bend forward from the hips with one leg stretched farther forward on the floor and, keeping your back straight, straighten both legs at the same time.
Cervical Myelopathy
Cervical myelopathy is a common degenerative spinal condition in the neck. Damage to the spinal cord, usually from compression of the cervical (neck) vertebrae, causes it. However, the disease is preventable, and you can live 70 years or longer without ever getting the disease.
Facet Joints and Crepitus
Facet joints are the pointy parts of your spine that you can sometimes see when you curve your back. Their job is to help your back stay aligned. There are two on each vertebra, one on each side. Cracking in the lower back, also called crepitus, is very common and happens whenever the facet joints move in or out of their normal position.
You may hear a crack or pop, and you also may feel grinding or pressure release, but it’s not usually painful. However, if you do feel pain when your back cracks, you may want to talk to your doctor.
Facet Arthropathy
Time and everyday movement may result in arthritis in the facet joints, also called facet arthropathy. The severity of facet arthropathy will vary from person to person. Unlike a herniated disc, the pain from facet arthropathy doesn’t normally radiate to other parts of the body. However, because these joints can swell, they may press on a few nerves, referring pain elsewhere.
Numbness and Tingling
Numbness and tingling in the limbs is a common sign that a disc is pinching your nerves. Pinched nerves may also cause muscle weakness. Because nerves running down the legs originate in the spine, tingling in the knees (paresthesia) can be another symptom of degenerative disc disease. However, paresthesia may also occur with injury and other conditions, including tendonitis, diabetes, gout and lupus. If tingling persists, talk to your doctor to determine its cause.
Pressure on nerves in the neck area can cause tingling in the neck or pain elsewhere. This is called referred pain. Tingling in the arm or hand or shoulder pain radiating down the arm to the thumb often starts in the spine.
Headache
Nerve compression in the neck from degenerative disc disease may cause cervicogenic headaches. Pain usually starts in the back of the head and may spread to the top of the skull and sometimes the temple. Pain behind the eyes is also typical. You may feel pain in the neck as well. Nausea, irritability and concentration difficulties are also common symptoms of cervicogenic headaches.
Degenerative Disc Disease Causes
Age
As we age, many of us will experience degeneration in our inter vertebral discs. According to a study published in Osteoarthritis and Cartilage, 90 percent of people 50 and over have some form of the condition. The condition only gets a label when degeneration causes pain.
Dry, Thin Intervertebral Discs
One of the most common causes of degenerative disc disease is the inter vertebral discs drying out. These discs are like hard jelly donuts with tough, fibrous outer rings and soft cores. When we’re young, they have lots of water in them, but as we age, they dry out. As they dry out, they get thinner. Thinning discs are less able to absorb shock, causing pain.
Common Treatments
Treatments for degenerative disc disease are usually conservative and start with the basics — exercise, stretching and physical therapy. Doctors usually recommend some over-the-counter medications such as ibuprofen or acetaminophen to help. Or they may prescribe muscle relaxants and narcotics.
As far as medications go, doctors often prescribe prednisone for arthritis. However, prednisone may cause many unpleasant and potentially dangerous side effects, such as weight gain, bruising, osteoporosis, increased blood pressure and cholesterol levels and diabetes.
Chiropractic manipulation or massage may provide relief for lower back pain without drugs or surgery. Transcutaneous electrical nerve stimulation (TENS) can dull the pain temporarily. Depending on your symptoms, your doctor may schedule you for an MRI or X-ray to check for bone and nerve damage. They may then schedule you for a spinal steroid injection to decrease inflammation.
Surgery for degenerative disc disease is usually a last resort when other remedies don’t offer relief. One surgical treatment for nerve pain in the back is burning the nerves in the spine. Surgeons will first numb the affected area and then insert a hollow needle containing a heated wire into your spine, burning the nerves causing the pain.
Preventing Degenerative Disc Disease
Many people would prefer to prevent degenerative disc disease and herniated discs naturally (herniated discs can heal on their own). A diet with nutrient-dense whole natural foods is essential to maintain a healthy spine. Staying hydrated will also help. Regular exercise will help keep your back strong, and gentle yoga can help improve your back’s flexibility. Good posturing is also key to preventing herniated discs.
Bone and Joint Health Supplements
There are many supplements that support joint health. The body naturally makes collagen, methylsulfonylmethane (MSM), glucosamine and chondroitin, but it doesn’t produce as much of these compounds as it ages. Supplements can help. Bone broth, fish oil and capsaicin have all shown in clinical studies to alleviate joint inflammation. Traditional remedies for joint health include Boswellia serrata, willow bark extract, cat’s claw and rose hips.
SEE ALSO

Tinea Pedis (Athlete’s Foot): Causes, Symptoms & Treatment
If you plan to take supplements to alleviate symptoms of degenerative disc disease, talk to your doctor first to determine whether they’re right for you. Also, for each supplement you plan to take, ask your doctor for their dose guideline. Follow your doctor’s dose guidelines over the ones listed below. If you don’t have access to a doctor, follow dose guidelines on supplement packaging.
Chondroitin Sulfate
Chondroitin sulfate is one of the most popular natural supplements for joint health. This compound is one of the main components of cartilage, which tends to break down as we age. The body makes chondroitin, but it makes less as we get older. The recommended daily dose is between 750 and 1,500 milligrams. It is best to divide these amounts into several smaller doses.
Glucosamine
Glucosamine is another component of cartilage and present in joint fluid. Research has shown that it has anti-inflammatory properties and may even help regrow cartilage. For D-glucosamine HCL powder, the recommended dose is up to 1,000 milligrams three times daily.
Collagen
Collagen is the most common type of protein in the body and is essential for healthy joints. Unfortunately, as we get older, we produce much less of it. Research has shown that collagen supplements can reduce inflammation in the joints as well as strengthen them. Collagen supplements (bovine, porcine, chicken and fish) are often available as powders, and it is ideal to take 2,500 milligrams two to four times per day.
Willow Bark Extract
Health-care practitioners have used willow bark medicinally for thousands of years to relieve joint pain and inflammation. Willow bark extract contains active ingredients similar to aspirin, as well as tannins, catechins and flavonoids, which have anti-inflammatory, antiseptic, analgesic and immune-boosting properties. Take between 400 and 1,600 milligrams daily.
Methylsulfonylmethane
Methylsulfonylmethane (MSM) is a compound with anti-inflammatory and antioxidant properties the body makes. MSM can alleviate symptoms of arthritis and keep your joints healthy. Take between 1,000 and 1,300 milligrams four times per day.
Boswellia Serrata
Boswellia serrata is a traditional Ayurvedic treatment that can help improve joint function. Its anti-inflammatory effects can help minimize pain, swelling and stiffness in the joints. Try taking 450 milligrams up to twice daily.
Fish Oil
The anti-inflammatory omega-3 fatty acids found in fish oil may relieve symptoms of arthritis as well as support heart and brain health. One study showed that taking 2.6 grams of omega-3s daily significantly improved symptoms in patients with rheumatoid arthritis. Take two capsules up to three times per day. Keep fish oil refrigerated and take with meals.
Pine Bark Extract
Pine bark extract is a powerful antioxidant with anti-inflammatory effects that may alleviate joint pain from degenerative disc disease. Take no more than 500 milligrams or one capsule daily.
Cat’s Claw
Cat’s claw is a vine from the rainforest of Peru that has shown clinical efficacy in the treatment of rheumatoid arthritis. Take 500 milligrams up to twice daily.
Other Bone and Joint Health Supplements
Capsaicin
Found in spicy peppers, capsaicin has shown efficacy as an analgesic. Capsaicin creams may alleviate joint and arthritis pain.
Rose Hips
Rose hips are edible fruit of the rose bush. Native Americans have used rose hips in traditional medicine for centuries. Studies have shown that rose hips, which have anti-inflammatory properties, can prevent certain proteins from degrading joint tissues.
The Bottom Line
Degenerative disc disease is a very common condition that affects many of us as we age. Regular exercise and maintaining a healthy weight can help prevent its onset. Supplements such as collagen, glucosamine and chondroitin can help alleviate its painful symptoms and help you live a fuller life. Talk to your doctor if you suspect you have this condition to determine the best treatment plan for you.



