Gingivitis: Symptoms, Causes & Treatment
Gingivitis
What is Gingivitis?
Gingivitis is a non-destructive periodontal disease caused by inflammation of the gingiva (tissues that surround and support the teeth). Inflammation could be caused by a buildup of plaque, a naturally occurring sticky film filled with bacteria. Plaque releases toxins that lead to irritation of the gums, which results in inflammation. It is a very common dental problem, and many people suffer from it at one time or another. Gingivitis is rare in children, but mainly begins during early childhood or puberty. It can occur and disappear throughout one’s lifespan.
An individual might be unaware that he or she has gingivitis since it can be a mild type of gum disease. It causes little or no pain. However, if left untreated, gingivitis can lead to periodontitis. This is more severe and may eventually cause loss of teeth.
One symptom of gingivitis is bad breath. Bad breath is caused by the same bad bacteria that cause gingivitis. Healthy gums are firm and tightly fitted around the teeth. They are pale pink in color. Once affected by gingivitis, gums become swollen and puffy and are dark red in color. Other symptoms of gingivitis include bleeding and tender gums. Do not ignore these signs as they could signify more serious problems.
Gum disease is linked to several health problems like heart disease and diabetes that affect the whole body. This gum disease can disappear in a few days so long as one practices good oral hygiene.
Types of Gingivitis
There are two main forms of gingival diseases:
- Dental plaque-induced gingival disease: This category is caused by malnutrition, plaque, medications and systemic factors.
- Non-plaque induced gingival lesions: This can result from fungus, virus infection or be caused by a specific bacterium. It can also be caused by a reaction to foreign bodies like dentures, systemic conditions like allergic reactions or genetic factors. Sometimes, there may be no specific cause.
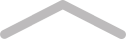
Gingivitis Symptoms
Swollen Gums
When gums are inflamed, they turn red and become sensitive to the touch because the gums are attacked by toxins released by plaque. These toxins cause irritation on the gum tissue. They pile up on the gum line, which many consider the main cause of gingivitis.
Dark Red Gums
Red gums is an obvious sign of gingivitis. They may also be dusky red. The color changes from the normal pale pink in healthy gums.
Receding Gums
Gum recession is common in many people with gingivitis. Recessed gums tend to reveal a bigger part of the tooth as compared to healthy gums. Thus, teeth appear longer than when compared to their size before the gum disease developed.
Bad Breath
Also known as halitosis. Chronic foul breath is the primary warning sign of gingivitis. According to the American Dental Association (ADA), bad breath indicates poor dental care. Foul breath may come in tandem with an unpleasant taste in the mouth. It could be triggered by the millions of bacteria in the plaque that produce smelly waste products.
Other Symptoms
A Pocket Between Tooth and Gum
A patch or area may develop between the tooth and gum. There may be several pockets in the mouth. Food particles may get into these pockets and cause the growth of bacteria. These bacteria may irritate the gum tissue and, if not treated, can lead to the development of an infection.
Pus Between the Tooth and Gum
Gingivitis can occur if a thick, yellow fluid builds up in the space between the tooth and gum. An individual who develops this fluid in the pocket between the tooth and gum may experience pain in case there is a buildup of pressure in the fluid. Pus forms if an infection occurs in the pockets between the tooth and gums. At this point, the infection could signify a periodontal abscess or gum abscess.
Tooth Pain or Sensitivity
When there is gum recession, a large part of the tooth becomes exposed, which makes the teeth become more sensitive to cold beverages and foods.
Bleeding Gums
People with gingivitis may have bleeding gums, especially when they brush or floss because the gum tissue is weak due to bacterial infection.
Loose Teeth
This refers to the way the teeth fit when a person bites down. It could indicate the presence of periodontitis.
Individuals who suffer from gingivitis may have one or all of these symptoms of gingivitis. One should see a doctor if they suspect the presence of any gum disease.
Who Can Get Gingivitis?
Groups that are at increased risk of developing gingivitis are:
- Individuals taking medication like cyclosporine and anti-epilepsy medicines
- Pregnant women or those taking birth control pills
- Individuals with poorly managed diabetes
Gingivitis Causes
Plaque Buildup
This typically comes as a result of poor oral hygiene. Plaque is a sticky film containing bacteria that accumulates between and around the teeth. The plaque forms when sugar and starch in food come into contact with bacteria found in the mouth. Once the plague forms, it triggers an immune response, which will eventually cause the destruction of gingival tissue.
The plaque should be removed on a daily basis because it rebuilds quickly. If it is not removed, the plaque hardens into tartar or calculus at the bottom of the teeth.
Hormonal Changes
These include the menstrual period, pregnancy, menopause and puberty. These changes may trigger the sensitivity and inflammation of the gums. This makes it easier for gingivitis to occur. It is vital that one improves their dental care while undergoing these physical changes.
Poor Oral Hygiene
Failure to brush or floss regularly puts an individual at a greater risk of developing the condition — it makes it easier for gingivitis to develop. However, one can easily avoid this issue.
Medications
Medications can also affect oral health. Some interfere with the flow of saliva, which has a protective role on teeth and gums. Some drugs like Procardia, Adalat and the anticonvulsant medication Dilantin can cause abnormal development of gum tissue.
Smoking
Tobacco use is a major risk factor related to gum disease and may decrease the possibility of successful treatment. Research shows that smokers are at a greater risk of developing gingivitis by up to 7 times that of non-smokers.
Chronic Diseases
Diseases like HIV, diabetes and cancer lower the body’s ability to defend itself from infections like gum disease. Patients with diabetes are more prone because it impairs the body’s ability to synthesize blood sugar.
Poor Nutrition
This deprives the body of beneficial health nutrients and makes it difficult for the body to protect itself from an infection like gingivitis. For example, vitamin C deficiency is linked to gum disease.
SEE ALSO
Pulmonary Embolism: Causes, Symptoms & Treatment
Family History of the Dental Disease
This can be a significant factor in the development of gingivitis. Children with a parent that had gingivitis are at a greater risk of developing the same. It can also manifest due to bacteria acquired during childhood.
Stress
Stress is associated with many health conditions like cancer and hypertension. It is also a risk factor for gum diseases. Stress makes it difficult for the body to combat and fight off infections, including gingivitis.
Preventing Gingivitis
Use of Anti-Gingivitis Toothpaste
One should use toothpaste that is able to get rid of plaque from the teeth and around the gum line.
Toothbrush Replacement
This should be done every three months once the bristles become worn out as they can only get rid of less plaque.
Good Oral Hygiene
Brush your teeth regularly. Brush in the morning and before heading to bed. It is also advisable to brush after a meal or snack. Floss at least once daily. Flossing before brushing allows the loose bacteria and food particles to wash away more easily.
Practicing Good Health Practices
Healthy habits like healthy eating and controlling blood sugar for individuals with diabetes is essential in managing and maintaining gum health.
Regular Dental Visits
Visiting a dentist regularly for cleaning keeps gingivitis away. Visits should occur in intervals of six to 12 months. Professional cleaning is essential for people with risk factors like smoking, dry mouth and medications. Annual dental x-rays can identify diseases not noticeable by the naked eye and also monitor any changes in a patient’s dental health.
Gingivitis vs. Periodontitis
Both gingivitis and periodontitis are types of periodontal disease. However, gingivitis is reversible, while periodontitis is not, due to the fact that periodontitis involves bone loss that cannot be recovered. Progressive and untreated gingivitis can develop into periodontitis.
Gingivitis Remedies and Supplements
Gingivitis Medications
Treatments that can fight against gingivitis include:
- Oral antibiotics: This can curb persistent areas of gum inflammation.
- Antiseptic mouthwash: Antiseptic mouthwash with chlorhexidine can help in disinfecting the mouth.
- Flap surgery: During this procedure, the gums are lifted back while tartar and plaque are removed from huge pockets. After, the gums are sutured in place to adjust well around the tooth.
- Bone and tissue grafts: These can be applied in case the teeth and jaw are severely damaged.
- Doxycycline: This antibiotic can prevent enzymes from triggering tooth decay.
Natural Supplements for Gingivitis
Aloe Vera
This is essential in dental health as it helps in getting rid of disease-causing bacteria found in the mouth. It is actually a popular ingredient in various tooth gels. As a dietary supplement, take 1,000 mg of aloe vera extract powder once daily with 8 oz of water or beverage of choice, or as directed by a physician.
Turmeric
Many regard turmeric as a superfood. It is effective in preventing gingivitis and keeping plaque at bay. This is largely thanks to its anti-inflammatory benefits. It has an active component called curcumin, a powerful anti-inflammatory agent with a powerful antioxidant effect. Take 1,000 mg of curcumin natural turmeric extract powder once a day. Take it along with water or a meal.
The Bottom Line
Gingivitis is a common dental problem that can cause bad breath and poor oral health. It is typically a result of the formation of plaque around the base of the teeth and on the gums. Poor dental health can lead to gingivitis, and the condition can also be triggered by health issues like diabetes and cancer. Treatment options for gingivitis include taking oral antibiotics, bone and tissue grafts and flap surgery, among many others. Natural remedies for gingivitis include taking aloe vera powder extract and turmeric powder extract.



