Peripheral Vascular Disease: Symptoms, Causes & Treatment
Peripheral Vascular Disease
What is Peripheral Vascular Disease?
Peripheral vascular disease (PVD) is a cardiovascular disorder in which blood circulation to the “peripheral” areas of the body, such as the arms and legs, is reduced. It can also impact blood flow to organs located in the torso such as the kidneys, stomach and intestines. This causes pain, fatigue, and tissue damage in those areas.
Signs of peripheral vascular disease can be subtle at first and worsen gradually. Muscle fatigue, changes in the appearance of skin on the arms and legs, and unusual sensations in the extremities can all signal problems with blood flow. Recognizing signs and addressing them early improves the long-term outlook. Many types of treatments are available including lifestyle changes, medication, surgery, and dietary supplements.
Types of Peripheral Vascular Disease
PVD, also called peripheral artery disease (PAD), is divided into two main types — occlusive and functional. Occlusive PVD occurs when a blood vessel becomes blocked and blood can’t travel through it freely. Functional PVD, on the other hand, happens when blood vessels don’t work properly.
Peripheral vascular disease isn’t just one standard disorder. There are several conditions that are considered to be an occlusive PVD including thrombophlebitis, deep vein thrombosis, and arteriosclerosis.
Like occlusive PVDs, a group of conditions also fall under the category of functional PVDs. These include rare diseases like Reynaud’s Syndrome, erythromelalgia, and acrocyanosis. Common conditions like varicose veins and chronic venous insufficiency also are examples.
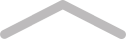
Symptoms of Peripheral Vascular Disease
About half of those who have peripheral vascular disease don’t notice symptoms at first. When signs are recognized, they most commonly involve the legs and are felt while engaging in physical activity like walking. Eventually, symptoms flare more frequently and can be felt even while resting.
Claudication
With PVD, oxygen-rich blood has a hard time reaching the distal areas of the body. Pain, cramping, or fatigue in one or both legs, also known as claudication, is the most common symptom of PVD. It usually happens when someone is engaging in activity such as walking and goes away after a few minutes of rest when the muscles reduce their need for oxygen. As PVD progresses, however, resting may not be enough to relieve the pain and fatigue.
Wounds and Ulcers
All tissue in the body relies on blood to deliver the oxygen and nutrients it needs. If an area is cut off from an adequate blood supply, cells become inflamed and eventually die. This can lead to skin ulcers, wounds, and gangrene on the legs or feet. While gangrene can lead to amputation, the risk of needing an amputation luckily remains low when people seek treatment for PVD.
Changes in the Appearance of Skin and Nails
In addition to ulcers and wounds, reduced blood flow can cause other visible skin changes. These include:
- A blueish tinge to the skin, especially the toes
- Reduced hair growth on peripheral areas like legs and arms
- Skin becomes thinner and may appear shiny
- Nails become thick and opaque
Impotence
Erections require an adequate supply of blood flow to the penis. When this doesn’t happen, as is the case sometimes with PVD, people might experience erectile dysfunction.
Odd Sensations in the Peripheral Areas
In addition to pain, fatigue, and cramping that comes with claudication, people with PVD might notice other unusual sensations in areas like the toes or fingers. They can feel cold, numb, tingly, or like they’re burning.
Complications
If left untreated, occlusive forms of PVD can lead to a heart attack, stroke, or pulmonary embolism. These serious and potentially fatal events happen when a blood clot or too much plaque build-up forms in the blood vessels and cuts off oxygen to vital organs.
Sometimes, though rarely, people may need all or parts of their legs or feet amputated as a result of gangrene.
Finally, walking and overall mobility can become challenging due to numbness, weakness, and/or pain in the legs.
Causes of Peripheral Vascular Disease
PVD happens when blood can’t pass through veins and arteries as it should. Something could be physically blocking the vessel, like a blood clot or fatty plaque. Or, the blood vessel could suddenly become narrow as a result of faulty signals from the brain. And in some people, the walls of the blood vessels become weak and simply can’t move the blood the way they used to. In other words, many things can bring about PVD.
Atherosclerosis
Atherosclerosis, or a buildup of plaque in the arteries, is the major cause of occlusive PVD. When plaque — a sticky substance made up of fat, cholesterol, calcium, and protein — accumulates in the blood vessels, they become narrow and blood can’t flow through as well. Risk factors for atherosclerosis (also called arteriosclerosis) include:
- Smoking
- Being overweight
- High cholesterol and/or triglycerides
- Having diabetes
- Elevated CRP levels (a marker of inflammation)
- Heavy alcohol use
- High blood pressure
- Advanced age
Physical Inactivity
Not only does an inactive lifestyle increase the chances of being overweight and developing diabetes, both of which are major risk factors for plaque buildup, it also contributes to poor function in peripheral veins. Varicose veins and blood clots, for example, are more common in sedentary adults.
Injury
Injury to a blood vessel increases the risk for plaque buildup, blood clot formation, and/or loss of function that can lead to peripheral vascular disease. Sometimes injuries are obvious like those that occur during surgery, getting an IV infusion, or having an accident. Others are less obvious. For example, the stress placed on blood vessels from chronically high blood pressure can damage them as well.
Other Causes
Functional PVD encompasses some diseases and syndromes that have nothing to do with plaque buildup, advanced age, or lifestyle choices. Reynaud’s disease, for example, more often affects young women and is triggered by cold and/or emotional stress. Causes and risk factors of other types of PVD include:
- Exposure to cold or very warm temperatures
- Genetics
- Emotional stress
- Certain medications
- Having another disease
Treatments for Peripheral Vascular Disease
PVD affects over 200 million people worldwide and the rates are expected to increase as people live longer.
Modifying the diet to improve cardiovascular health is also important. This includes eating foods that help achieve a healthy weight, reduce blood pressure, lower cholesterol, and control diabetes.
More movement also improves cardiovascular health and symptoms of PVD, especially claudication. Exercise therapy usually lasts 12 weeks with the goal of increasing walking time. Those who comply with exercise plans set by their healthcare team can improve their walking time by 150%. Unfortunately, exercise and movement become very difficult for some people with claudication, especially diabetic women, and results of this type of therapy vary.
Managing stress levels and making an effort to sleep well also lowers inflammation that contributes to atherosclerosis and reduces triggers for some functional PVDs.
Medication
Lifestyle changes are necessary to improve peripheral vascular disease but medication may also be required. Which to use depends on the factors contributing to the condition in the first place. Drugs can be prescribed to help lower cholesterol and blood pressure. Blood thinners may be needed to prevent blood clots. If a person has diabetes, medication to stabilize blood sugar and insulin levels is often needed.
Surgery
At some point, a person may need surgery to manage PVD. Surgical options include angioplasty, or inserting a catheter into one or more blood vessels to increase blood flow. A bypass surgery requires more invasive technique. With a bypass, a blood vessel from one area of the body is used in another area to reroute blood flow.
SEE ALSO
Rhabdomyolysis: Symptoms, Causes & Treatment
Supplements for Peripheral Vascular Disease
Supplements can be useful for maintaining a healthy cardiovascular system. If you take medication or have a health condition of any kind, it’s important to ask your doctor which supplements are safe for you.
Coenzyme Q10
Coenzyme Q10, also called ubiquinone, is a potent antioxidant linked to several health benefits. Research shows that it can be particularly useful for supporting cardiovascular function by potentially lowering blood pressure, improving atherosclerosis, and providing energy to cardiac cells. This coenzyme might also exert a beneficial effect on blood sugar levels and inflammation which in turn could improve diabetic conditions. If you’re already taking medication, it’s especially important to ask your doctor before using COQ10 as they may not interact well. As a supplement, it is recommended to ingest 50 to 200 milligrams of COQ10 at your and your physician’s discretions.
L-Arginine
L-Arginine is an amino acid that helps your athletic endurance and heart functions. The body produces some on its own and gets more through food, especially meat. In the body, L-arginine acts as a precursor to nitric oxide. Nitric oxide helps to relax and widen blood vessels, allowing blood to flow through them more efficiently. As a dietary supplement, take 750mg of L-arginine one to three times daily on empty stomach, or as directed by physician.
L-arginine may be beneficial for some people with cardiovascular issues but harmful for others. For this reason, please consult with your doctor before taking it. If you have liver issues, are taking ACE inhibitors or diuretics and have kidney problems or you recently had a heart attack, you should not take this supplement.
Hesperidin
This supplement, other than boosting your mood and immune system, supports your circulatory health. It contains a chemical found in certain citrus fruits called bioflavonoids. If not directed differently by your doctor, take 500 milligrams of hesperidin twice a day with food and water. If you have a history of low blood pressure and cardiovascular tissue damage do not take this supplement.
Do not take this hesperidin two weeks before surgery. If you are pregnant or nursing, talk to your doctor on the potential issues it might cause.
Nattokinase
Nattokinase is an enzyme that comes from a Japanese food made of boiled soybeans, called natto. This enzyme has protein-digesting effects that helps improve circulation and prevent the formation of blood clots. As a result, studies show that it can help prevent conditions including peripheral vascular disease.
As a dietary supplement, take 100 milligrams of nattokinase one to three times daily, or as directed by a physician. Avoid this product if you are allergic to soy or are taking aspirin, ACE inhibitors, diuretics, blood clotting medication or beta blockers.
Hawthorn Berry Extract
Thanks to its rich phytonutrient content, hawthorn berry extract may exert a protective effect on the cardiovascular system by reducing blood pressure, improving cholesterol and strengthening vessel walls. As a dietary supplement, the regular dosage is 1200mg, twice a day, unless your physician says otherwise. Pregnant women or people on heart medication should avoid hawthorn berry.
Green Tea Extract
Green tea contains antioxidants (polyphenols to be specific) that help support health in lots of different ways. Studies link the compounds in green tea extract to better blood sugar control, lower cholesterol, healthy blood pressure, and weight management. While it makes a beloved beverage, green tea also comes in a powdered extract. As a dietary supplement, take 500mg of green tea extract one to two times daily. DO NOT use more than 1000mg in a day. Not intended for use longer than 3 months, as prolonged use of high amounts of EGCG (a type of polyphenol) may cause liver or kidney damage.
The Bottom Line
Peripheral vascular disease is a blood circulation disorder that most often results from a blockage in the blood vessels. Fatty plaque or blot clots are common examples of obstructions within veins and arteries. Peripheral vascular disease most commonly affects older adults, especially those who smoke, have diabetes, high cholesterol, high blood pressure, or any other factor that puts their cardiovascular function at risk. Symptoms progress gradually and often includes fatigue, pain and numbness in the legs. If untreated, a person may lose the ability to walk or develop severe wounds on the legs and feet.
In some cases, rather than an occlusion, wrong signals from the brain or a problem with the blood vessel lining can cause them to become too narrow or remain too dilated. This is called functional PVD and can be caused by other conditions, medications, or genetics.
Lifestyle changes, medication, surgery, and dietary supplements can all be part of the overall treatment plan for peripheral vascular disease. The sooner a person seeks medical help, the better the outcome is likely to be.



